The Labeling Exercise 2-2 Reference Manual provides essential guidelines for accurate specimen labeling, ensuring clear and consistent identification to enhance laboratory efficiency and compliance with standards.
1.1 Overview of the Manual
The Labeling Exercise 2-2 Reference Manual serves as a comprehensive guide for specimen labeling, detailing requirements for collection, preparation, and shipping. It outlines standardized procedures to ensure accurate identification and compliance with laboratory protocols, providing a clear framework for users to follow in various healthcare settings.
1.2 Purpose of the Labeling Exercise
The purpose of the Labeling Exercise 2-2 is to teach accurate specimen labeling, ensuring clear identification and compliance with laboratory standards. This exercise trains users in best practices, reducing errors and enhancing workflow efficiency. It focuses on correct label formats, patient data accuracy, and adherence to regulatory requirements for reliable test outcomes.
1.3 Target Audience for the Manual
The Labeling Exercise 2-2 Reference Manual is designed for students, healthcare professionals, and laboratory staff. It serves as a training tool to equip users with essential skills for accurate specimen labeling and processing. The manual is particularly useful for those new to laboratory practices and those seeking to refine their expertise.

Key Components of the Labeling Exercise 2-2 Reference Manual
The manual covers specimen preparation, standardized labeling formats, and shipping procedures. It provides detailed guidelines for accurate identification and handling of samples to ensure reliable test results.
2.1 Specimen Requirements and Preparation
The manual outlines specific requirements for specimen collection, including types of containers, recommended volumes, and storage conditions. It also details patient preparation steps, such as fasting or timing, to ensure sample integrity for accurate laboratory testing and analysis.
2.2 Labeling Guidelines and Standards
The manual establishes standardized labeling formats, emphasizing clear patient identification, specimen type, and collection date/time. It ensures compliance with regulatory standards, requiring consistent and legible labels to prevent errors and maintain traceability during laboratory processing and analysis.
2.3 Shipping and Handling Procedures
The manual details proper shipping and handling procedures, including secure packaging, temperature control, and labeling for transport. It emphasizes maintaining specimen integrity, preventing leakage, and ensuring compliance with safety regulations during transit to preserve sample accuracy and safety.

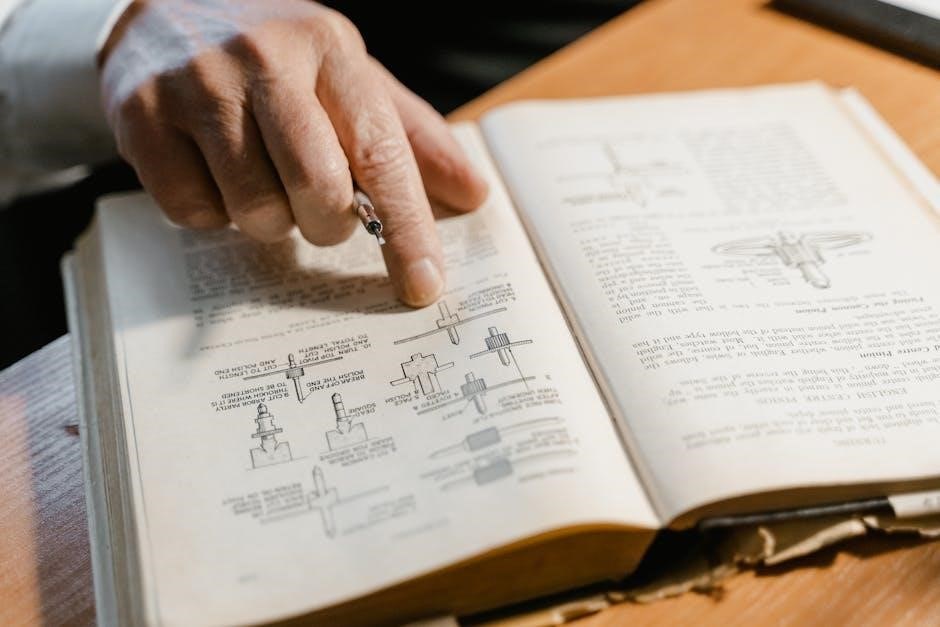
The Labeling Process: Step-by-Step Instructions
This section provides a detailed, step-by-step guide on specimen labeling, from collection to completion, ensuring accuracy and compliance with laboratory standards and best practices.
3.1 Collecting and Identifying Specimens
Proper specimen collection involves using appropriate containers, ensuring accurate patient identification, and adhering to specific collection times. Clear labeling with patient ID, date, and specimen type is essential for accurate processing and testing, minimizing errors in laboratory workflows.
3.2 Using Standardized Labeling Formats
Standardized labeling formats ensure consistency in specimen identification by including patient ID, specimen type, collection date, and time. This approach minimizes errors, ensuring accurate processing and compliance with laboratory standards, and maintains specimen integrity throughout the testing process. These elements are crucial for traceability and efficiency in laboratory workflows.
3.3 Avoiding Common Labeling Errors
Common labeling errors include incorrect patient ID, illegible handwriting, and mismatched specimen types. To prevent these, always double-check labels against requisitions, use barcode systems for accuracy, and ensure all information is clear and complete. Adhering to standardized formats and guidelines helps minimize errors and ensures reliable specimen identification and processing.

Exercises and Quizzes for Practical Application
The manual includes interactive exercises and quizzes to test knowledge and practical skills, ensuring users can apply labeling guidelines accurately and confidently in real-world scenarios.
4.1 Types of Labeling Exercises Included
The manual features a variety of exercises, including specimen identification, label formatting, and practical scenarios. These exercises focus on patient identification, specimen types, and handling procedures, providing hands-on experience to enhance accuracy and consistency in real-world laboratory settings.
4.2 Role of Quizzes in Reinforcing Learning
Quizzes serve as interactive assessments to reinforce understanding of labeling standards. They test knowledge of specimen identification, formatting, and compliance, ensuring retention of key concepts. Regular quizzes help identify knowledge gaps and provide practical examples to improve accuracy in real-world laboratory scenarios.
4.3 Evaluating Competence Through Assessments
Assessments evaluate practical skills in specimen labeling, ensuring adherence to guidelines. They use real-world scenarios and standardized criteria to measure accuracy and consistency. Regular evaluations identify strengths and areas for improvement, while self-assessment tools empower learners to refine their techniques and maintain high standards of competence in laboratory procedures.
Best Practices for Effective Specimen Labeling
Best practices include using clear, consistent labels, standardized formats, and accurate patient identification. Ensure specimen type and collection details are precise to maintain compliance and patient confidentiality.
5.1 Importance of Clear and Consistent Labels
Clear and consistent labels ensure accurate specimen identification, reducing errors and enhancing laboratory efficiency. They provide essential patient and specimen information, promoting compliance with regulatory standards and maintaining patient safety throughout the testing process.
5.2 Using Technology for Accurate Labeling
Technology enhances labeling accuracy by utilizing barcode systems, automated printers, and software integration. These tools ensure consistency, reduce human error, and streamline the labeling process. Integration with Laboratory Information Systems (LIS) further improves efficiency, enabling real-time data synchronization and traceability of specimens.
5.3 Maintaining Patient Confidentiality
Maintaining patient confidentiality is crucial in specimen labeling. Secure labels with limited access ensure only authorized personnel can view patient information. Compliance with regulations like HIPAA and secure storage of labeled specimens further safeguard privacy, protecting sensitive data from unauthorized disclosure.

Troubleshooting Common Labeling Issues
This section addresses frequent labeling challenges, such as illegible text or missing information, and provides solutions to correct errors promptly, ensuring accurate specimen identification and reliable test results.
6.1 Identifying and Correcting Labeling Errors
This section outlines methods to detect labeling mistakes, such as mismatches in patient/specimen identification or incomplete information. It provides step-by-step guidance on re-labeling or correcting errors, ensuring accuracy and compliance with laboratory standards to prevent test delays or misinterpretation of results.
6.2 Resolving Discrepancies in Specimen ID
This section provides strategies to address mismatches in specimen identification, such as verifying patient data, cross-referencing with collection records, and using barcode scanning to ensure accurate and reliable specimen ID resolution, minimizing errors and delays in laboratory testing.
6.3 Managing Missing or Damaged Labels
This section outlines procedures for handling missing or damaged labels, including re-labeling specimens with verified data, documenting the issue, and notifying lab staff. It emphasizes the importance of maintaining accurate records and ensuring specimen integrity to prevent delays or mix-ups in testing processes.

Updates and Revisions to the Reference Manual
The manual undergoes periodic updates to reflect new standards, technologies, and best practices. Users are encouraged to check official sources regularly for the latest revisions.
7.1 Sources of Updated Information
Updates to the Labeling Exercise 2-2 Reference Manual are available through official websites, professional organizations, and digital platforms. Users can access revised guidelines via newsletters, training modules, or dedicated portals to ensure compliance with the latest standards and practices.
7;2 Importance of Staying Current
Staying current with updates ensures compliance with evolving standards, reduces labeling errors, and enhances laboratory efficiency. Outdated practices may lead to inaccuracies, inefficiencies, or non-compliance, potentially compromising patient safety and test reliability. Regular updates help maintain accuracy and adapt to new technologies or regulations in specimen labeling.
7.3 How to Access Revised Guidelines
Revised guidelines can be accessed through the official website, automated email notifications, or the laboratory’s intranet. Users are encouraged to regularly check for updates and subscribe to alerts to ensure they always have the most current version of the labeling manual.
Integration with Laboratory Information Systems (LIS)
The manual details how to integrate labeling processes with LIS, ensuring seamless connectivity for accurate data transfer and efficient specimen tracking within laboratory workflows.
8.1 Linking Labels to Electronic Records
Linking labels to electronic records ensures accurate and efficient specimen tracking within laboratory workflows. Barcode scanning integrates with LIS, enabling real-time data updates and reducing manual entry errors. This process ensures patient data accuracy, streamlines lab operations, and maintains compliance with regulatory standards for reliable test outcomes and patient care.
8.2 Automating Labeling Processes
Automating labeling processes involves using software and barcode scanners to streamline specimen identification. This reduces manual errors and enhances efficiency. Integration with LIS ensures real-time data updates, improving traceability and compliance with regulatory standards. Automated systems also support batch processing, minimizing delays and optimizing lab workflow.
8.4 Ensuring Compatibility with LIS
Ensuring compatibility with LIS involves integrating labeling systems with electronic health records. This ensures seamless data exchange and accuracy. Standardized formats and barcode scanning enhance compatibility, while regular updates and system checks maintain synchronization. Compatibility is crucial for efficient lab operations and accurate specimen tracking.
Benefits of the Labeling Exercise 2-2 Reference Manual
The manual enhances specimen handling accuracy, streamlines lab workflows, and ensures compliance with regulatory standards, improving overall efficiency and reliability in laboratory operations and patient care.
9.1 Improved Accuracy in Specimen Handling
Proper labeling ensures specimens are accurately identified, minimizing mix-ups and ensuring correct association with patient data. This clarity reduces errors, leading to precise test results and reliable patient care outcomes, as outlined in the reference manual.
9.2 Enhanced Efficiency in Lab Workflow
The Labeling Exercise 2-2 Reference Manual streamlines laboratory operations by providing clear guidelines for specimen labeling. This reduces delays in processing, minimizes manual sorting, and ensures specimens are quickly matched to test requests, improving overall workflow efficiency and productivity in the lab setting.
9.3 Compliance with Regulatory Standards
The Labeling Exercise 2-2 Reference Manual ensures adherence to regulatory standards by providing clear labeling protocols. This compliance minimizes legal risks and ensures accurate test results, meeting requirements from agencies like CLIA and CAP. Proper labeling helps maintain patient safety and avoids penalties associated with non-compliance, ensuring lab accreditation and operational integrity.

Challenges and Limitations of the Manual
The manual may present complexity for new users, requiring additional training. Updates can lag behind new technologies, and human error remains a risk despite clear guidelines provided.
10.1 Common Difficulties in Labeling
Common difficulties include human error, complex labeling procedures, and specimen mix-ups. Ensuring accurate patient identification and adhering to standardized formats can be challenging. Additionally, maintaining consistency across multiple samples and avoiding illegible handwriting are frequent issues that require careful attention and proper training to mitigate.
10.2 Limitations of the Manual
The manual may not cover all unique laboratory scenarios, requiring additional guidance for specialized tests. It focuses on general practices, potentially lacking depth for complex or less common labeling situations. Updates may lag behind rapidly evolving technologies or regulatory changes, necessitating supplementary resources for complete accuracy.
10.3 Strategies to Overcome Challenges
Regular updates to the manual ensure alignment with evolving standards. Cross-referencing with supplementary guides addresses unique scenarios. Interactive tools, such as quizzes and diagrams, enhance understanding. Collaboration with experts and feedback mechanisms help refine practices. Providing examples of complex labeling situations improves applicability and user confidence.

Future Trends in Specimen Labeling
Emerging technologies like RFID and automation are transforming specimen labeling, enhancing accuracy and efficiency. These innovations ensure compliance with future regulatory standards and practices.
11.1 Emerging Technologies in Labeling
Emerging technologies such as RFID tagging, advanced barcode scanning, and automated labeling systems are revolutionizing specimen labeling. These innovations improve accuracy, reduce manual errors, and enhance traceability, ensuring seamless integration with laboratory information systems for efficient workflow management and compliance with future standards.
11.2 Impact of Automation on Labeling
Automation significantly enhances labeling efficiency by minimizing human error and accelerating the process. Advanced systems, such as barcode scanners and labeling software, ensure consistent and accurate specimen identification. This streamlines workflow, reduces manual labor, and integrates seamlessly with laboratory information systems, improving overall compliance and operational performance.
11.3 Evolving Standards and Practices
Evolving standards and practices in specimen labeling reflect advancements in technology and regulatory requirements. Updates often include new formatting guidelines, enhanced patient privacy measures, and integration with digital systems. Staying informed about these changes is crucial for maintaining compliance and ensuring accurate, efficient specimen identification in laboratory settings.